Spending to support older people must rise now… and fast
A Fabian Society review of recent evidence and projections reveals the scale of future spending pressures and the level of unmet need today
When policy makers discuss the ‘ageing society’ or ‘demographic change’ is sounds distant and theoretical, as if it is something we can postpone worrying about until never-ending austerity is over. Nothing could be further from the truth. Disability-related need is rising very rapidly, right now – as this year’s NHS crisis is demonstrating. We need a new vocabulary to express this urgency.
The first call on new spending should be to adequately fund ‘business as usual’ as the number of older people with support needs grows. But in recent elections, politicians have failed to say this directly or to set out spending plans that provide adequately for maintaining the existing public offer. The temptation is always to propose new entitlements, before saying how much will be needed to pay for current provision as needs and costs rise. For example, in 2017 Labour pledged £3bn for social care in England (for adults of all ages) but listed a range of new entitlements that much of this money would need to pay for.
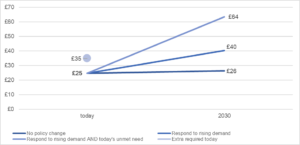
For this research the Fabian Society has reviewed a range of published estimates and projections for the rising costs of supporting older people over the next decade, on a business-as-usual basis. This is the first time projections across so many different areas of activity have been brought together in one place. Our conclusion is that, across all forms of provision, public spending on older people with support needs in England needs to rise from £25 billion today to at least £40 billion in 2030. This is a rise from 1.2 per cent of GDP to 1.8 per cent of GDP, which is the equivalent of a tax increase in England of £7 billion today (the rest of the extra money would be generated by tax revenues rising in line with economic growth). The service-by-service breakdown is presented in the table below.
Extra spending requirements for each service area by 2030 to respond to rising levels of need (2017/18 prices)
| Billion | |
| NHS continuing care (all ages) | £4.4 |
| Social care: home care | £3.5 |
| Social care: care homes | £2.4 |
| NHS intermediate care | £1.5 |
| Disability benefits | £1.2 |
| Social care: assessment and other services | £1.0 |
| Supported housing | £0.8 |
| NHS free nursing care (all ages) | £0.5 |
| Equipment and adaptations (all ages) | £0.2 |
| TOTAL | £15.6 |
The scale of the spending required is illustrated vividly when put in terms of annual increases. To spend £40 billion by 2030, it will take an annual real increase of 3.8 per cent – which will typically translate into a rise of 5 to 7 per cent a year in cash terms. Spending increases on this scale are needed this year and every year.
What’s more these figures are relatively cautious. Most of the estimates take into account rising levels of disability (although worryingly this does not appear to be the case for the DWP’s disability benefit projections). However, we’ve used variants based on relatively optimistic scenarios for population health: future health-related needs could be much higher if current health trends persist. This means that a significant focus on public health and preventative interventions will be needed even for spending on this scale to be sufficient.
The figures also assume that carers continue to provide the same proportion of care and support as they do today – which will require a very large increase in the amount of care provided by older people’s partners, adult children and other relatives and friends. This might prove impossible for family and friends to supply.
These estimates are also based on existing patterns of service provision. In other words, they roll-forward the totally inadequate level of support seen today – including the huge recent cuts in the numbers receiving home care, the inadequate size of many care packages, the under-funding of care homes and the under-supply of supported housing. For example, even though these spending increases are high, they would not provide enough money for commissioners to fully meet the ambitions (and legally binding obligations) of the Care Act’s framework for assessment and eligibility. In other words, they do not take account of the extra spending that is already required now, to fully meet the needs of older people today.
Public spending scenarios for support and care for older people in England (£ billion, 2017/18 prices)
To illustrate the scale of the challenge the Fabian Society has developed estimates of the extra spending required to fully meet the needs of older people requiring support today, under current financial entitlements. In total we estimate that £10 billion extra is required to meet present need, with a breakdown as follows:
- £5 billion – the cost of providing support to 1.2 million low/mid-income older people who aren’t receiving help with essential daily tasks including washing, dressing and eating.
- £1.5 billion – the extra spending needed for NHS rehabilitation services to support all older people who could benefit
- £1.3 billion – the cost of adequately funding council-paid care home places, to ensure sufficient quality and stop unfair cross-subsidies and top-up charges
- £1.2 billion – a cautious estimate of the money to tackle isolation, promote wellbeing and step in early to prevent needs arising
- £0.9 billion – a cautious estimate of the extra annual spending needed to bring the supply of specialist older people’s housing more into line with other countries
To increase spending over the next decade to both address these shortfalls and respond to rising demand would cost billions more. The Fabian Society estimate for the cost of meeting all need in 2030 is around £60 billion. This is 2.8 per cent of GDP. Increasing spending to this level would be equivalent to a tax rise of £24 billion today. In annual terms it is equivalent to a real rise in spending of 7.5 per cent a year.
This article is an extract from A fresh start: rethinking support and care for older people in England, a research paper being presented to a Fabian Society summit on older people’s care and support on Monday 19 March 2018.

